Living with Alzheimer’s
By: Pastor Doug Schweyer
On January 20, 2020, I was diagnosed by a doctor as having the beginning stages of Alzheimer’s disease. Right away the doctor insisted on taking my driver’s license away. She said I had the right to protest by applying to the Government Board with a $ 700.00 cheque not refundable! I decided based on the results of the battery of tests I had just taken that I would not pass the written and road tests required so I accepted the verdict. Joyce drove home and has been the driver for us ever since.
So, what is Alzheimer’s disease? It is a form of dementia; in fact, it makes up about 70% of all persons in Canada who have been identified with dementia. The other 30% are diagnosed with other symptoms with other names. Usually, Alzheimer’s has a component of short-term memory loss, increasing forgetfulness, and a general slowing down of the normal brain functions. In its early forms, it may not be recognized but, as it progresses, these and other symptoms become more recognizable.
Since the diagnosis that I had beginning stages of Alzheimer’s disease, Joyce as my caregiver and I have taken three of the mini-courses offered by the Alzheimer’s Society of Hamilton. As a result of those courses, I have been asked to join a group sponsored by the Hamilton-Haldimand Group. This group is made up of five people in various stages of Alzheimer’s disease. Our mandate is to make recommendations to the larger group about possible programs that could help those with Alzheimer’s.
This is not an easy task! We are just beginning to get acquainted and discover that we all are different people, each with different experiences of the way this disease affects us and how we relate to the community. Part of the difficulty of designing how to help one another is the different ways each person experiences life after the diagnosis. Many do not want to talk about it or even face the diagnosis. Others have no difficulty describing their feelings about the disease but again those experiences are not necessarily shared by others. Our progress is slow.
For instance, today we had a virtual meeting scheduled but the link to the meeting was slow in coming and most of us did not show. So, we cancelled the meeting and went our separate ways without much ado. We will meet again next week. Very relaxed! Time does not mean as much to many who have Alzheimer’s as perhaps it once did.
What seems common to most however is a desire to have people, especially close family and friends, continue to treat us the same as before the diagnosis, in other words, as normal human beings, even if there is some difference in how we respond. The stages of the disease will come soon enough, although there is some evidence that some people can keep relatively normal activities for some years. In the group I am involved with, one person is still in the early stages and has been for fourteen years!
Dr. Sanjay Gupta has written a book titled Keep Sharp: Build a Better Brain at Any Age. He is a brain surgeon and an experienced media commentator. In this latest book, Gupta suggests that, in addition to the five senses of sight, smell, taste, touch, and hearing, there are as many as six more: a sense of balance, a sense of pain, a sense of temperature, a sense of time, a sense of internal needs of the body, a sense of your body parts and where they are and what they are doing. Dr. Gupta suggests that we know more about the brain than many people think. He believes that we can improve brain function by eating healthy, keeping active physically, sleeping at a usual time and more.
Almost two years have now passed since my diagnosis. Not much has changed in my journey. However, there is some change in my involvement with Alzheimer’s and the community. I am presently involved in two groups, each with a slightly different emphasis. In both, the goal is to help the community understand the disease better. Look for some reporting in the community soon. Also, look for more in this Newsletter.
That message is that Alzheimer’s disease has as many faces as people who have it. We are all at different stages of the disease and cannot be pigeon-holed into a preconceived idea or formula. Of course, there are some characteristics that can be identified but that can only be done as one gets to know each individual who has the disease. It is a complex disease and presents varied forms in every individual.
About the Author: J Douglas Schweyer is a retired pastor of the Evangelical Lutheran Church in Canada, now a member of Trinity Lutheran Church in Hamilton. Presently along with his wife of almost 60 years they live in St. Elizabeth Village, a Seniors Community in Hamilton.

Living with Alzheimer’s: A Care Partner’s Perspective
By: Joyce Schweyer
Our family kept asking, what’s with dad? He shuffles his feet, walks very slow and bent over . . . what’s going on? This was my wake-up call to face the fact that in the last 6 months or more, changes were happening with Doug. I thought: It’s time to see our family doctor – maybe it’s the medication he’s on.
At his doctor’s appointment, Doug went through a series of tests. He tried his best but couldn’t fool the doctor and she arranged for an appointment with a geriatrician. We went, like lambs to the slaughter, after all it’s nothing serious that can’t be fixed.
We were separated right from the start: Doug with the doctor, and me with her assistant. Boy, could she ask questions! I couldn’t figure out why she was asking me all these questions, it was Doug that had the appointment. Very personal, I felt very disloyal to my husband (I figured it out later). Then we switched and the doctor gave me the results of her assessment: ALZHEIMER’S.
Okay. Now, my usual reaction to hard news is to go very quiet until I’m able to take it in! Ha-ha- no time. All four of us got back together to give the diagnosis to my wonderful, smart husband. When he heard the verdict, the look in his eyes for a few seconds was fear and ‘help me’. I felt so helpless. Then, the other hard knock came. By law, the doctor had to immediately report to the motor vehicle department that he no longer had a licence to drive. With this news, the look in Doug’s eyes was one of relief. He knew it was time, there had been too many close calls in the past months. So, I was now the only reluctant driver.
As we walked out of his appointment, we were in a daze. We held hands and promised each other that we are in this together and for the long hull. I drove out of the parking building, for the first time, and have been driving us around ever since.
Adjusting to living with Alzheimer’s
Our family is there for us. The Alzheimer’s Society is the best and has given us much-needed help. We were able to take a Beginner’s Course about living with dementia (First Steps), which is just what we needed. We called the LHIN who sent an Occupational Therapist to assess what we needed to help in the house. I have a love-hate relationship with the toilet handlebars. We are to call when we need more help. I even found out that Doug can keep his opinions and mouth shut when I do something stupid while driving!
It’s taken us some time to really come to terms with how our life has changed. After working in nursing homes for many years, I know that arguing with somebody who has dementia will not help. That’s hard, so I tell Doug I can’t argue with you, and that works for now. I pray to God that he is with us, to guide me to be patient. Doug tries so hard to keep active and help me around the house, he loves to vacuum with our Dyson vac. I only have great respect and love for him- my husband for nearly 60 years. He can’t remember what I told him two minutes ago, but I bet he could get up and preach a sermon for 15 minutes!
About the Author: For nearly 60 years, Joyce Schweyer has been the wife, friend, companion, and now care partner to Doug Schweyer. Joyce calls her role as a pastor’s wife “the best job I have ever had, with many ups and downs, pastor Doug and I have always worked together, and so it will always be.”
What Does My Diagnosis Mean?
By: Phyllis Fehr
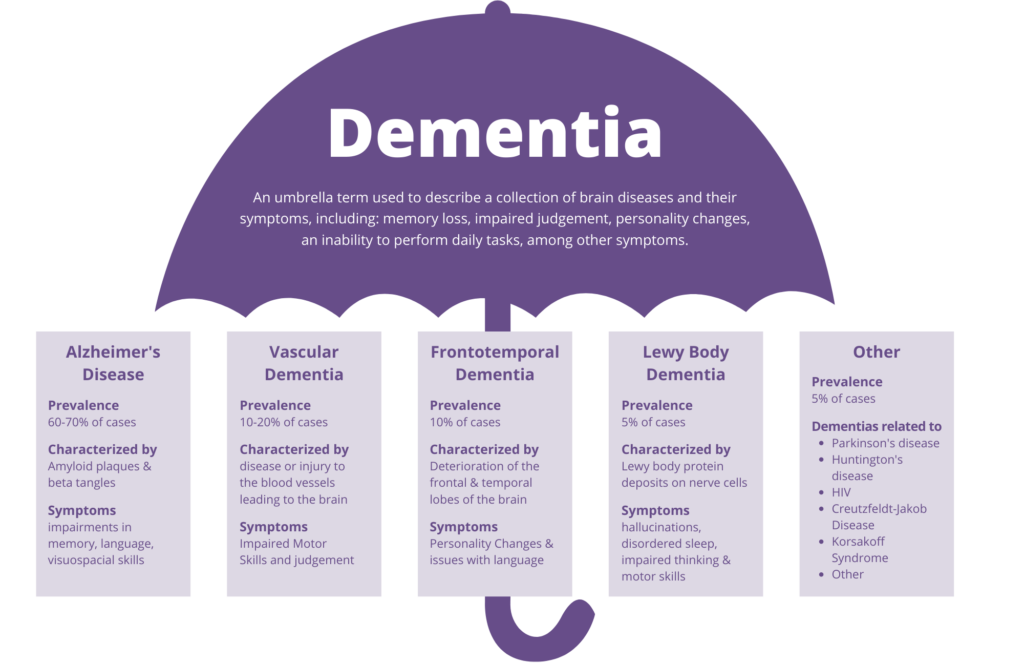
People often ask: What is the difference between Alzheimer’s disease and Dementia?
Dementia is an umbrella term used to describe numerous neuro-cognitive diseases. You may hear people say that they don’t have dementia, they have Alzheimer’s disease, Lewy Body Dementia, Vascular Dementia, or many others.
The truth is that people living with all of the mentioned and other diagnoses ALSO live with dementia.
The symptoms of dementia can vary and may include:
- Experiencing memory loss, poor judgment, and confusion
- Difficulty speaking, understanding, and expressing thoughts, or reading and writing
- Wandering and getting lost in a familiar neighborhood
- Trouble handling money responsibly and paying bills
- Repeating questions
- Using unusual words to refer to familiar objects
- Taking longer to complete normal daily tasks
- Losing interest in normal daily activities or events
- Hallucinating or experiencing delusions or paranoia
- Acting impulsively
- Not caring about other people’s feelings
- Losing balance and problems with movement
Does knowing what type of dementia I have matter?
You may also hear people describe their diagnosis simply by saying that they have dementia. They do not say and may not know what their specific diagnosis is. Is this important? YES, IT DOES MATTER!
It is important that you know and understand what type of dementia you have in order to move forward and develop an understanding and care plan that is best for you and your loved ones. Common symptoms and treatments will vary from diagnosis to diagnosis, so the more information you know, the better! It is useful for medical professionals to have in-depth knowledge and understanding of your diagnosis in prescribing medications and to recommend non-medical treatment options, such as vitamins and lifestyle changes that are tailored specifically to what you are going through. It may also be helpful for you or your family members to become connected to education or support groups that are most specific to your diagnosis.
What should I do if I suspect I might have dementia?
First off, don’t panic! The first thing you should do is make an appointment with your doctor. It is important to be self-aware but not to self-diagnose. Know that what you are experiencing may be a variety of things and the sooner whatever it is can be assessed by a qualified medical professional, the better off you are going to be!
For individual support and guidance about symptoms you may be experiencing or to learn about how to better support somebody who lives with dementia, please contact your local Alzheimer’s Society. (Hamilton office: 905-529-7030, www.alzda.ca)
About the Author: Phyllis Fehr is a wife, mother, grandmother and great grandmother to a blended family. Her career was as a Registered Nurse in both Intensive Care and Cardiac settings, as well as a sexual assault nurse examiner. Since being diagnosed with Alzheimer’s disease, Phyllis has become an international advocate for people living with dementia.

The 3 C’s Following My Diagnosis
By: Debbie Keay
My diagnosis of young-onset Alzheimer’s did not come as a shock. What caught me off guard was the emotional rollercoaster that I endured over the course of the next 18 months. Even though I was a Social Worker and thought I had all the answers, my positive attitude took a little more than a nosedive.
As we know Alzheimer’s is a silent disability. You may share your diagnosis with some, others not. Most of my family and friends found out about my diagnosis just recently, three years after my diagnosis from an article where I shared my story on the front page of the newspaper! A private person, I have lived my life – “some information for some, some for none, some for everyone.”
My diagnosis experience included unexpected and extreme feelings. They stemmed from caring for seven family members over the last 40 years and my misconception about dementia. As mentioned previously, it took me 18 months to adjust to my circumstances. There are still challenges and disappointments, but I have ways of dealing with them. I call my coping strategies:
My 3 C’ s – Can’t, Challenged, Can.
When I was first “given” my diagnosis- “taken” from me was the life I knew. Despite my extreme feelings of loss, I was encouraged not to think about the things I “can’t” do and encouraged to focus on the “can’s”. This well-intended suggestion was easier said than done and did not work for me initially. All the focus on my disability was the “CAN’TS”. All my past seemed to have been wiped away, my present and my future. Addressing my losses was instrumental in my self-care. I needed to mourn all my losses. Those supporting me would say: “There is a light at the end of the tunnel”. I would respond: “But, I am the caboose and cannot see the tunnel”.
Not only was I having to adapt to my new circumstances, I had to adapt to the different way people around me were seeing/treating me. Those finding out about my diagnosis were at a loss of what to say and do, and relationships started to fade.
Slowly, things started to change. Once addressing and accepting my “CAN’TS”, I began to focus on my “CHALLENGES”. Not easy, but I guess that’s why they are called challenges, and this is when something wonderful started to happen. In facing my “challenges”, I began succeeding at mini accomplishments and my confidence became elevated, leading me to tackle more difficult challenges. I had not realized how much I had allowed dementia to take from me.
The more I succeeded at adapting to the “challenges”, I started to focus on the “CAN’S”. The more “CAN’S” done, the more my old self returned. While my life today is not the same as what it was three years ago, or what I envisioned my life would be like, I can honestly say that I am enjoying moments of my life today. I feel a sense of purpose. I feel a sense of accomplishment. Most importantly, in living with dementia, I still feel like me.
Tips That May Ease Your Journey
- When diagnosed ensure you have a care team (doctors, pharmacists, etc.) that listen to you and understand dementia. Don’t be afraid to ask every question that comes to your mind. (E.g.: Are there medications that may help with symptoms?)
- Connect with your local Alzheimer’s Society. We cannot do this alone. Friends and family will be able to help, but their level of understanding may be minimal even with best intentions. The Alzheimer’s Society has an excellent education program for those with dementia and their Circle of Care/Care Partners – all free of charge!
- Join a support group even if you are shy and private like I am. Being supported by people who know and understand what you are experiencing is amazing. To be able to laugh and enjoy life despite the diagnosis, is a gift you will give to yourself. You may find your “cans” far outweigh your “cant’s”/”challenges” put together.
- Reach out. The Alzheimer’s Society offers free counselling as do many physicians’ offices. There are also crisis phone lines to help in the middle of the night if you feel “punky”. Remember it is okay to feel what you feel. Some will spend thousands of dollars to get their cars fixed, why not treat yourself to that same care.
- Try not to beat yourself up on the things you are unable to do or that you are disappointing others. This was a big issue for me. Feelings of being useless, guilty because you cannot meet the expectations of others, not being a “super-duper”, always there for others (not bragging here LOL). You may question your lack of participation, withdrawing, feeling emotionally depleted. Remember, these may be symptoms of your dementia.
- You also all know this: get restful sleep, eat well, exercise, eliminate stressful situations and avoid negative people (I call them “negatoids.”) Find a time to be with yourself, your quiet place. Remind yourself that you still have lots to offer.
- Find a confidant(s) that can be that listening ear and won’t downplay what you are going through. So many people say “You don’t look like you have dementia.” or “I lose my keys all the time, those senior moments.”
- Some individuals have a faith connection. Trust it, even though you might think you’ve lost it. Someone will find you that will help you reconnect. We do not have to do all the work. We need to be patient with ourselves and find our “cognitive ramp”, a term one of my support group members use. If a person has lost a leg, they get a prosthetic; if a person has lost sight, they utilize a cane or a seeing eye dog; if a person uses a wheelchair, they need ramps to get in and out of buildings. Our disability is unseen, so we need “cognitive ramps”, people who can help us with our thinking when we need it or ask for it. I call them nudges. A beautiful friend is my computer mainframe, giving me reminders, putting my ideas to paper, etc.
- Educate yourself. There are free courses the Alzheimer’s Society offers. If searching the internet, be cautious of the resources, some are very outdated. Discern what is valid. Speaking to people with dementia and connecting to respected/academic/gov’t agencies will ensure recent info is available and recognized as good resources.
- Identify yourself not by what you can do, being a spouse, mother, career person, sports athlete, etc… but by who you are – Caring, intelligent, educated, loving, kind, encouraging, life experienced, and far more than you probably think you are. It’s the inside you that really matters.
- There was a book entitled “Don’t Sweat the Small Stuff”. You need to learn to prioritize things. For me I do not worry and do not sweat the small stuff but I sure to take care of it because if I do not take care of the small stuff (because I forget due to my dementia), the small stuff turns to HUMONGOUS STUFF LOL. Remember though what works for one person, may not work for another. Each person’s journey is unique. Take all that you learn and take the very best that works for you and your journey. You will be amazed at how the reservations you may have had about this disability will be so much lessened.
- Stay involved, try new things. For example: Perhaps you would like to share your thoughts and ideas with this newsletters? . . .Hint, Hint. Think big. I plan on going skydiving in the spring.
About the Author: Debra Anne “Debbie” Keay lives with her cat, rabbits and birds. Artistic, a continual learner, environmentalist, and more, Debbie began advocating 40 years ago for causes close to her heart. Debbie was diagnosed 3 years ago with early-onset Alzheimer’s Disease. She now uses her experience to advocate for community inclusion for those who live with dementia.

